1204
Views & Citations204
Likes & Shares
INTRODUCTION
Cervicogenic headache is a referred pain condition where in a pain source in the cervical spine is experienced as a headache. Its diagnosis and pathophysiology have remained controversial. The clinical criteria for its diagnosis have undergone several modifications since the time it was first described. We provide an overview of the diagnosis of cervicogenic headache, our hypothesis on its pathogenesis, and the management of cervicogenic headache.
Diagnostic criteria
The diagnosis of cervicogenic headache based on clinical criteria has been revised several times since its original description in 1980s [1]. It was initially defined as a unilateral headache associate with evidence of cervical involvement through provocation of pain by movement of the neck or by pressing the neck; concurrent pain in the neck, shoulder, and arm; and reduced range of motion of the neck with or without other features. These criteria were nonspecific and did not validate the nature of the cervicogenic source. It was modified in 2013 to include cervical spondylosis in the imaging criteria and clinical response to diagnostic blockade to form the guidelines for International Classification of Headache Disorders (ICHD-3-beta) [2]. The prevalence of CGH is reported to range from 1-4% in the general population and contributes to more than 17% of all severe headache types [3-5]. Recent studies using ICHD-3 criteria estimated it to be around 22% of all headaches [6]. About 88% of patients with cervical myeloradiculopathy are noted to have associated cervicogenic headaches [7].
Differential diagnosis
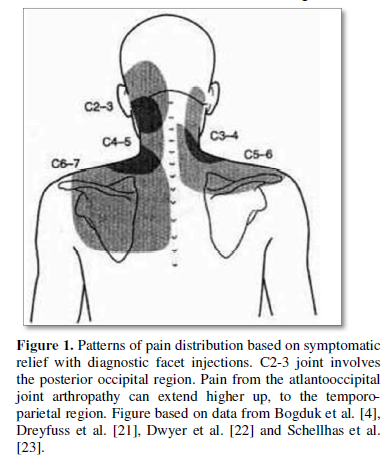
The term cervicogenic headache encompasses all sources of pain from the cervical spine and usually is associated with mechanical neck pain. The pain generator for mechanical neck pain as well as headache could be varied including paraspinal muscles and ligament injury, cervical disc and spondylotic changes such as uncovertebral arthropathy and facet arthropathy [8]. The pain origin from upper cervical facets is mediated through cervical nerve roots and extends cranially generally up to the coronal suture as demonstrated in illustrations (Figures 1 and 2).
The differentials of cervicogenic headache include paroxysmal hemicrania, migraine cervicale and Barre’s Syndrome. Paroxysmal hemicrania, unlike CGH is characterized by several attacks (>5 a day) of severe periorbital pain, usually responsive to indomethacin. Clinical evaluation of patients with cervicogenic headache should include a detailed history for symptoms such as timing and frequency of attacks, location, triggering mechanisms, and autonomic symptoms such as photophobia, conjunctival injection, visual disturbances and nausea. Clinical examination must include provocative maneuvers such as Spurlings and L’Hermitte’s signs and evaluation of trigger points to differentiate conditions such as occipital neuralgia.
The clinical criteria for cervicogenic headache differentiate it from some of the close mimics such as tension-type headache and migraine.
Originally, on the anatomic basis of upper cervical nerve roots’ (C1 to C3) convergence to the spinal segment of trigeminal nucleus, CGH origin was believed to be limited to the upper cervical segments [9,10]. It is however established now that CGH symptoms are noted to arise from the lower cervical spine as well [11]. There is no definitive pathoanatomic mechanism in the literature supporting this observation. We present our hypothesis, based on our analysis of cervical neural anatomy, radiological findings and clinical results with various treatment strategies.
Review of relevant cervical anatomy
Occipital region and area extending up to the coronal suture innervated by occipital nerves and the greater auricular nerve can directly contribute to headache. The frontal and temporal region CGH however, is mediated through convergence to the trigeminal nucleus. It is important to understand the anatomic detail of cervical spine innervation to appreciate the origin of CGH associated with spondylosis. The duramater and extradural structures of the cervical spine are innervated by corresponding cervical nerve roots via the anterior and posterior primary rami. The anterior primary ramus along with the sympathetic branches gives rise to sinuvertebral (SV) nerves that innervates the anterior duramater, cervical discs, atlantoaxial ligaments and clival dura. The SV nerve runs in the lateral to medial direction through the foramen, into the spinal canal extradurally, in association with venous plexus and arterioles. It provides the nociceptive and sympathetic innervation to the dura, posterior longitudinal ligament (PLL) and the cervical discs. The innervation of the SV nerve extends caudally up to 3 adjacent levels as demonstrated in previous cadaveric studies [12]. This provides one possible mechanism of CGH origination from the lower cervical spine, on the basis of trigeminocervical convergence. We speculate that the CGH nociception in spondylotic cervical spine is mediated through the sinuvertebral nociceptive and sympathetic innervation of the anterior duramater and posterior longitudinal ligament (PLL). The mechanisms as such could include compression at the narrow foraminal entry zone, dural stretch of varied etiologies such as cervical stenosis, kyphosis, spondylotic changes and associated segmental cerebrospinal fluid (CSF) entrapments [13]. Similarly, the posterior primary rami of the cervical nerve roots innervating the zygopophyseal joints and posterior musculature can also mediate CGH.
Management
Neurointerventional anesthetic blocks and/or radiofrequency neurotomy of nociceptive sources including lateral atlantoaxial joints, greater occipital nerve, cervical nerves and zygopophyseal joints have all shown to be beneficial in treating CGH [14-17]. Surgical treatment with both anterior and posterior approaches for cervical spondylosis associated cervicogenic headaches have been evaluated by numerous studies [6,7,18-20]. The anterior surgical approaches in general have demonstrated more substantial and durable pain relief compared to posterior cervical approach. We surmise that the posterior surgical techniques may only provide an indirect decompression of the richly innervated anterior dura and the PLL, which are more frequently the source of pain.
It is important to evaluate for the source of CGH before pursuing a surgical treatment. Careful evaluation of cervical imaging with appropriate trial of neurointerventional anesthetic blocks is necessary to differentiate the origin of the pain between the possible structures such as the cervical disc, facet joints, cervical nerves and the duramater.
CONCLUSION
Cervicogenic headache arises from varied etiologies including spondylotic changes such as disc degeneration, uncovertebral hypertrophy and zygopophyseal joint arthropathy. Recent guidelines help diagnose CGH based on both clinical and imaging criteria. First line conservative treatment options include use of muscle relaxants, rehabilitation of posterior neck musculature and interventional pain techniques. Surgical options may be considered in persistent, severe cases when associated with radiculopathy or myelopathy. Anterior surgical approach to address cervical spondylosis associated CGH seems to be a more effective and durable method, in contrast to posterior surgical operations. Removal of PLL as well as adequate uncovertebral and foraminal decompression may optimize headache relief with an anterior surgical approach.
DISCLOSURE
The authors have not received or will receive benefits for person or professional use from a commercial party related directly or indirectly to the subject of this manuscript. The study and the preparation of the manuscript were supported by a commercial party related to the subject of the manuscript.
1. Sjaastad O, Saunte C, Hovdahl H, Breivik H, Grønbæk E (1983) Cervicogenic headache. An hypothesis. Cephalalgia. 3: 249-256.
2. ICHD-3 (2018) The classification - 11.2.1 Cervicogenic headache. The International Classification of Headache Disorders. 3rd edn.
3. Evers S (2008) Comparison of cervicogenic headache with migraine. Cephalalgia 28: 16-17.
4. Bogduk N, Govind J (2009) Cervicogenic headache: an assessment of the evidence on clinical diagnosis, invasive tests and treatment. Lancet Neurol 8: 959-968.
5. Sjaastad O (2008) Cervicogenic headache: Comparison with migraine without aura; Vågå study. Cephalalgia 28: 18-20.
6. Shimohata K, Hasegawa K, Onodera O, Nishizawa M, Shimohata T (2017) The clinical features, risk factors, and surgical treatment of cervicogenic headache in patients with cervical spine disorders requiring surgery. Headache 57: 1109-1117.
7. Schrot RJ, Mathew JS, Li Y, Beckett L, Kim KD, et al. (2014) Headache relief after anterior cervical discectomy: Post-hoc analysis of a randomized investigational device exemption trial. J Neurosurg 21: 217-222.
8. Cyriax J (1938) Rheumatic headache. Br Med J 2: 1367-1368.
9. Kerr FWL (1961) A mechanism to account for frontal headache in cases of posterior-fossa tumors. J Neurosurg 18: 605-609.
10. Hunter CR, Mayfield FH (1949) Role of the upper cervical roots in the production of pain in the head. Am J Surg 78: 743-751.
11. Diener HC, Kaminski M, Stappert, Stolke D, Schoch B (2007) Cervical disc prolapse may cause cervicogenic headache: Prospective study in patients undergoing surgery. Cephalalgia 27: 1050-1105.
12. Edgar MA, Nundy S (1966) Innervation of the spinal dura mater. J Neurol Neurosurg Psychiatry 29: 530-534.
13. Bartsch T, Goadsby PJ (2003) The trigeminocervical complex and migraine: Current concepts and synthesis. Curr Pain Headache Rep 7: 371-376.
14. Lord SM, Barnsley L, Wallis BJ, Bogduk N (1994) Third occipital nerve headache: A prevalence study. J Neurol Neurosurg Psychiatry 57: 1187-1190.
15. Ehni G, Benner B (1984) Occipital neuralgia and the C1-2 arthrosis syndrome. J Neurosurg 61: 961-965.
16. Sjaastad O, Fredriksen TA, Stolt-Nielsen A (1986) Cervicogenic headache, C2 rhizopathy and occipital neuralgia: A connection? Cephalalgia 6: 189-195.
17. Persson LCG, Carlsson JY, Anderberg L (2007) Headache in patients with cervical radiculopathy: A prospective study with selective nerve root blocks in 275 patients. Eur Spine J 16: 953-959.
18. Liu H, Ploumis A, Wang S, Li C, Li H (2017) Treatment of cervicogenic headache concurrent with cervical stenosis by anterior cervical decompression and fusion. Clin Spine Surg 30: E1093-E1097.
19. Riina J, Mathew JS, Li Y, Beckett L (2009) The effect of an anterior cervical operation for cervical radiculopathy or myelopathy on associated headaches. J Bone Joint Surg Am 91: 1919-1923.
20. Liu JJ, Cadena G, Panchal RR, Schrot RJ. Kim KD (2016) Relief of cervicogenic headaches after single-level and multilevel anterior cervical diskectomy: A 5 year post hoc analysis. Global Spine J 6: 563-570.
21. Dreyfuss P, Michaelsen M, Fletcher D (1994) Atlanto-occipital and lateral atlanto-axial joint pain patterns. Spine 19: 1125-1131.
22. Dwyer A, Aprill C, Bogduk N (1990) Cervical zygapophyseal joint pain patterns. I: A study in normal volunteers. Spine 15: 453-457.
23. Schellhas KP, Smith MD, Gundry CR, Pollei SR (1996) Cervical discogenic pain. Prospective correlation of magnetic resonance imaging and discography in asymptomatic subjects and pain sufferers. Spine 21: 300-312.
24. Foerster O (1933) The dermatomes in man. Brain 56: 1-39.
25. Cooper G, Bailey B, Bogduk N (2007) Cervical zygapophysial joint pain maps. Pain Med 8: 344-353.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- International Journal of Diabetes (ISSN: 2644-3031)
- BioMed Research Journal (ISSN:2578-8892)
- Journal of Otolaryngology and Neurotology Research(ISSN:2641-6956)
- Journal of Cancer Science and Treatment (ISSN:2641-7472)
- Journal of Blood Transfusions and Diseases (ISSN:2641-4023)
- Journal of Carcinogenesis and Mutagenesis Research (ISSN: 2643-0541)
- Chemotherapy Research Journal (ISSN:2642-0236)